When can I walk upstairs normally after TKR?
Article Updated: 09/02/2023
Walking Upstairs Post-Op
Throughout my extensive career as a physical therapist specializing in total knee replacements, I’ve observed a consistent pattern: the 10-week post-operative mark often serves as a significant milestone for patients. Around this time, many find themselves capable of walking upstairs in what can be described as a ‘normal’ manner. But what does ‘normal’ really mean in this context?

Walking upstairs ‘normally’ is more than just a subjective feeling; it’s a measurable achievement. It means you can confidently place one foot on each step, adopting a step-over-step walking pattern. This is a far cry from the initial post-operative weeks, where each step can feel like a monumental task. During this early phase, patients are generally advised to adhere to the “up with the good, down with the bad” stepping pattern, a method we’ll delve into later.
Reaching the 10-week mark is not just about physical readiness; it’s also about mental preparedness. The fear of re-injury or exacerbating pain can be a significant barrier to resuming normal activities, including stair climbing. That’s why it’s crucial to consult with your physical therapist and surgeon to ensure you’re not only physically ready but also mentally prepared to tackle stairs again.
It’s worth noting that individual experiences can vary. Factors such as age, overall health, and adherence to physical therapy protocols can influence the speed of your recovery. Therefore, the 10-week guideline is not a one-size-fits-all solution but rather a general timeframe that most patients can aim for.
Why Descending Stairs is More Painful
While the journey to walking upstairs post-surgery is a significant milestone, it’s often accompanied by a surprising revelation: descending stairs can be more challenging, and sometimes even painful. This counterintuitive experience leaves many patients puzzled. Why would going down be harder than going up?
The answer lies in biomechanics. When you descend stairs, the knee experiences an increase in shear force, a type of force that acts parallel to the surface of the joint. This shear force amplifies the pressure along the surgical incision site, making each step a potential discomfort zone. The mechanics of walking downstairs involve your knee extending over your heel, which results in an increased anterior shear force and heightened patellar compression. These biomechanical factors combine to make the act of descending stairs more strenuous on your newly operated knee.
Understanding the biomechanics is not just academic; it has practical implications for your recovery. Being aware of the forces at play can help you approach stair descent more cautiously, perhaps by using handrails or other assistive devices initially. It also underscores the importance of adhering to your physical therapy regimen, which often includes exercises specifically designed to strengthen the knee and improve its ability to handle shear forces.
Moreover, if you find that you’re still experiencing significant discomfort while descending stairs even after the 10-week post-op period, it’s crucial to consult with your healthcare team. Persistent pain could be a sign of underlying issues that may require further evaluation and possibly adjustments to your treatment plan.
Understanding “Up with the Good, Down with the Bad”
One of the first phrases you’ll likely encounter during your stair-climbing journey post-surgery is “Up with the good, down with the bad.” While it may sound like a simple mantra, it encapsulates a fundamental principle of post-operative mobility. So, what does this phrase actually mean, and why is it so crucial to your recovery?
The phrase serves as a mnemonic to help you remember which leg should lead when ascending or descending stairs. In the context of knee replacement surgery, “the good” refers to your non-surgical leg, while “the bad” refers to your surgical leg. When you’re going upstairs, your non-surgical leg should take the first step, acting as the leader. Your surgical leg will then follow, essentially being pulled up by the strength of your non-surgical leg. This minimizes the stress and strain on your newly operated knee.
Conversely, when you’re descending stairs, the roles reverse. Your surgical leg takes the lead, allowing your non-surgical leg to bear the brunt of your body weight and control the descent. This method is designed to distribute the forces involved in stair navigation optimally, reducing the risk of injury or strain to the surgical site.
Adhering to this principle is not just about physical technique; it’s also a mental tool. The phrase serves as a constant reminder to be mindful of your movements, especially in the early stages of recovery when the surgical site is most vulnerable. By internalizing this simple yet effective rule, you’re setting yourself up for a smoother, safer recovery journey.
Utilizing a Walker for Stair Climbing
For many patients recovering from a total knee replacement, a walker serves as an invaluable aid, especially when it comes to navigating stairs. However, using a walker on stairs is not as straightforward as it might seem. So, how should you position your walker for optimal safety and support while climbing stairs?
The general guideline is to place the walker sideways, on the side opposite to the handrail. This positioning allows you to use the handrail for additional support while keeping the walker stable. If your staircase is equipped with handrails on both sides, it’s advisable to use the handrail that is opposite your surgical leg. This setup provides a balanced distribution of weight and force, minimizing stress on your surgical knee.
But what if your staircase only has one handrail? In such cases, the walker should be positioned on the side opposite to the handrail. This arrangement ensures that you can still use the handrail for extra support while maintaining the walker’s stability. It’s a setup that maximizes safety while accommodating the limitations of your environment.
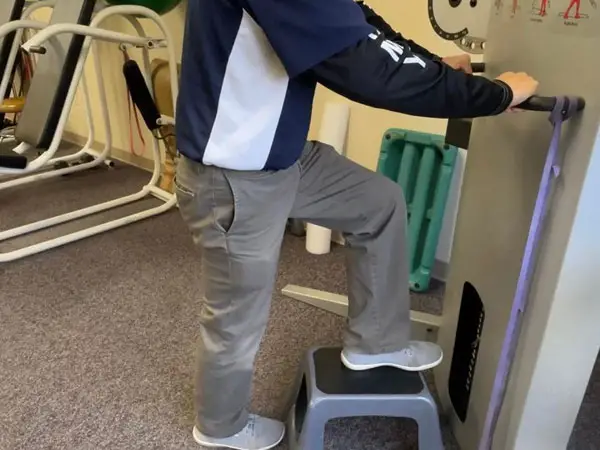
Using a walker for stair climbing is not just about positioning; it’s also about technique. Proper technique involves placing the walker on the step first, followed by your good leg, and finally your surgical leg. This sequence ensures that the walker and your stronger leg bear the brunt of your body weight, reducing strain on your surgical knee.
Remember, the goal is not just to get up and down the stairs but to do so in a manner that promotes healing and prevents injury. Therefore, always consult your physical therapist for personalized guidance on using a walker for stair climbing during your recovery.
The Benefit of a Second Walker
As you progress through your recovery journey, you’ll find that convenience and practicality become increasingly important. One tip that many patients find invaluable is the use of a second walker, specifically positioned upstairs. Why would you need a second walker, you might ask? The answer lies in the simple yet impactful benefit of convenience.
Having a second walker upstairs eliminates the cumbersome task of carrying your primary walker up and down the stairs each time you need to change levels. This not only saves you time but also reduces the risk of accidental slips or falls, which could be detrimental to your recovery. It’s a small investment that pays off in a big way, enhancing your mobility and independence during this crucial healing period.
Now, where can you find a second walker without breaking the bank? Fortunately, there are several cost-effective options. Local consignment shops often carry medical supplies, including gently used walkers. Medical supply depots are another option, offering a range of walkers that can fit various budgets. Don’t overlook charitable organizations like Goodwill or the Salvation Army, as they often receive donations of medical equipment, including walkers.
Before making a purchase, it’s advisable to consult your physical therapist for recommendations on the type of walker that would best suit your needs. Different walkers come with various features, such as wheels, seats, and storage compartments. Your therapist can guide you in choosing a walker that complements your primary one, ensuring that you have the best tools at your disposal for a successful recovery.
Choosing the Right Support: Walker, Cane, or Crutches
Once you’ve undergone a total knee replacement, the type of support you use in the initial stages of recovery can significantly impact your healing process. The three most common options are walkers, canes, and crutches. Each has its own set of advantages and limitations, and choosing the right one is crucial for a smooth and safe recovery.
Immediately after surgery, a walker is often the go-to choice for most patients. Walkers provide unparalleled support and stability, making them ideal for the initial post-operative phase. During the first 10 days following surgery, it’s common for patients to experience rapid fatigue, often due to factors like blood loss and low iron levels. A walker can help mitigate these issues by providing a stable platform that reduces the risk of falls or additional strain on the surgical site.
Crutches, on the other hand, require a considerable amount of upper body strength and coordination. While they offer more mobility than a walker, they are generally not recommended for older patients or those who are heavier. The reason is simple: the risk of falling or putting undue stress on the surgical knee outweighs the benefits of increased mobility.
After the initial 10-day period, a cane becomes a viable option for many. By this time, you’ve likely regained some strength and confidence in your surgical leg, making a cane a suitable choice for added support without the bulkiness of a walker. Canes are particularly useful for navigating tighter spaces and offer a good balance between support and mobility.
Ultimately, the choice between a walker, cane, or crutches should be made in consultation with your healthcare team. Your physical therapist can provide personalized recommendations based on your specific needs, ensuring that you choose the most appropriate support for your recovery journey.
Summary
In this comprehensive guide, we’ve explored various aspects of navigating stairs after a total knee replacement surgery. From understanding when you can walk upstairs ‘normally’ to the biomechanics that make descending stairs more challenging, this article aims to equip you with the knowledge you need for a smooth recovery. We’ve also delved into practical tips like using a walker and the benefit of having a second one. Whether you’re using a walker, cane, or crutches, choosing the right support is crucial, and this article provides insights to help you make an informed decision.
Recommended Reading
How much does physical therapy cost after a total knee replacement?
Phyiscal therapy cost varies greatly across locations and service providers. In this article we will examine the cost of physical therapy services for three different patients. One patient has traditional Medicare part B insurance. The second patient has no health...
3 Pros & Cons of Bilateral Knee Replacement
Having a bilateral knee replacement on the same day vs different days depends largely on your surgeon's assessment of your condition and current clinical research. A 2020 study suggested that patients receiving a same day bilateral knee replacement were not more...
Best shoes to wear after knee replacement
Best shoes to wear after knee replacement surgery:This article is specifically written to help you choose the best shoes to wear after knee replacement surgery when you return home. This information is focused on house-shoes and day 1 to week 6 post op.Click here to...
NEW Orthotics After Knee Replacement
Do You Need New Orthotics After Knee Replacement Surgery? Often, patients who receive a total knee replacement will have previously been prescribed custom orthotics. Custom orthotics may help reduce stress at the knee joint in the months or years before knee surgery...
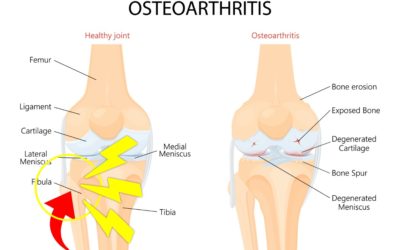
Pain on the Outside of Knee After Total Knee Replacement
Experiencing pain on the outside of knee is common among individuals who have had a total knee replacement. 1. Fibular Head (Outside of Knee) The long skinny bone that runs along the outside of your lower leg is called the Fibula. This bone is not directly involved...
Cupping Therapy After Total Knee Replacement
Although the risk of major medical complications attributed to cupping therapy is low, the efficacy of cupping therapy is poorly associated with post surgical care and total knee replacement scar tissue mobilization.Cupping Therapy Research As of March 21, 2022 a...