Overview of Spinal Stenosis
1. What is spinal stenosis
Spinal stenosis is a condition characterized by the narrowing of spaces within the spine, leading to increased pressure on the spinal cord and nerve roots. The spine consists of vertebrae that protect the spinal cord, nerve roots branching out from the cord, and various structures that support the body.
The narrowing in spinal stenosis can occur in different areas of the spine, including:
- The spinal canal: This is the hollow space within each vertebra that houses the spinal cord and nerve roots.
- The canals at the base or roots of nerves branching out from the spinal cord.
- The openings between vertebrae, through which nerves exit the spine and extend to other parts of the body.
There are four main regions of the spine: the cervical spine (neck), thoracic spine (upper back), lumbar spine (lower back), and the sacrum and coccyx (tailbone).
Spinal stenosis most commonly develops in the lumbar spine and cervical spine. The condition can occur gradually over time, and it may be caused by various factors.
It is important to note that anyone can develop spinal stenosis, but the likelihood increases with age. Older individuals are more prone to age-related changes in the spine, such as the thickening of ligaments or the growth of bone spurs.
Although age is a significant risk factor, spinal stenosis can also affect younger individuals who are born with a narrow spinal canal or who have experienced spinal injuries.
Common symptoms of spinal stenosis depend on the location of the narrowing within the spine. In the lower back, symptoms may include pain in the lower back, radiating pain or ache in the buttocks and legs, numbness or tingling in the legs and feet, and weakness in the legs and feet. On the other hand, spinal stenosis in the neck can cause symptoms such as neck pain, numbness or tingling in the arms and hands, and weakness in the hands, arms, or fingers.
Diagnosing spinal stenosis involves a comprehensive evaluation of symptoms, medical history, and physical examination. Medical professionals may also employ imaging tests like X-rays, MRI scans, or CT scans to assess the condition of the spine and confirm the diagnosis.
Treatment options for spinal stenosis can vary depending on the severity of symptoms and the individual’s overall health. Non-surgical approaches often include physical therapy, pain management techniques, and the use of assistive devices to alleviate discomfort and improve mobility. In more severe cases, surgery may be recommended to relieve pressure on the affected nerves or spinal cord.
If you suspect you may have spinal stenosis or would like more information about the condition, it is advisable to consult with a healthcare professional who can provide a proper diagnosis and guide you towards the most appropriate treatment options.
2. What are the symptoms of spinal stenosis
The symptoms of spinal stenosis can vary depending on the location and severity of the narrowing in the spine. In some cases, individuals may not experience any symptoms, while others may develop noticeable signs of the condition. Common symptoms of spinal stenosis include:
- Pain: Individuals with spinal stenosis may experience pain in the affected area of the spine. In the case of lumbar spinal stenosis, pain can manifest in the lower back, while cervical spinal stenosis may cause neck pain. The pain may be intermittent or persistent.
- Radiating pain: When spinal stenosis leads to compression of the nerves, individuals may experience radiating pain that extends from the affected area to other parts of the body. For instance, in lumbar spinal stenosis, the pain may radiate from the lower back into the buttocks and down the legs. Similarly, cervical spinal stenosis can cause radiating pain from the neck to the shoulders, arms, and hands.
- Numbness or tingling: Compression of the nerves can result in sensations of numbness or tingling in the extremities. This can occur in the legs and feet in cases of lumbar spinal stenosis or in the arms and hands with cervical spinal stenosis.
- Weakening of muscles: Spinal stenosis can lead to muscle weakness in the affected areas of the body. This weakness may manifest as difficulty in gripping objects, reduced strength in the arms or legs, or a general sense of decreased muscle function.
- Changes in bowel or bladder function: In some instances of severe spinal stenosis, individuals may experience difficulties with bowel or bladder control. This can include problems with urinary or fecal incontinence, an urgent or frequent need to urinate, or difficulty initiating urination.
- Sexual dysfunction: Spinal stenosis can also affect sexual function in some cases. Both men and women may experience a decrease in sexual desire or performance due to nerve compression in the spine.
It is important to note that symptoms can vary from person to person, and not all individuals will experience the same combination or severity of symptoms. Some individuals may have mild symptoms that do not significantly impact their daily lives, while others may experience more pronounced symptoms that affect mobility and overall quality of life.
If you are experiencing any of these symptoms or suspect you may have spinal stenosis, it is crucial to consult with a healthcare professional for a proper diagnosis and appropriate treatment options. Early detection and management of spinal stenosis can help alleviate symptoms and prevent further progression of the condition.
3. How is spinal stenosis diagnosed
Diagnosing spinal stenosis involves a comprehensive evaluation by a healthcare professional. The diagnostic process typically includes a combination of the following:
- Medical history: The healthcare provider will inquire about your symptoms, their duration, and any factors that may worsen or alleviate them. They will also ask about your medical history, including any previous spine-related issues or injuries.
- Physical examination: A physical examination allows the healthcare provider to assess your range of motion, muscle strength, reflexes, and any signs of nerve dysfunction. They may perform specific tests to elicit symptoms or evaluate your ability to walk or maintain balance.
- Imaging tests: Various imaging techniques can provide detailed images of the spine to confirm the presence of spinal stenosis. These may include:
X-rays: X-ray images can reveal changes in the bones, such as bone spurs, that may be contributing to spinal stenosis. However, X-rays do not provide a direct view of the nerves or spinal cord.
Magnetic Resonance Imaging (MRI): An MRI scan uses powerful magnets and radio waves to generate detailed images of the spine. It can visualize the spinal cord, nerve roots, and surrounding tissues, helping identify areas of compression or narrowing.
Computed Tomography (CT) Scan: A CT scan combines X-ray images taken from different angles to create cross-sectional images of the spine. It can provide detailed information about the bone structures and help identify any abnormalities or narrowing of the spinal canal.
Based on the results of these diagnostic tests, the healthcare professional can determine whether spinal stenosis is the cause of your symptoms and develop an appropriate treatment plan. It is essential to consult with a qualified healthcare provider for an accurate diagnosis, as other conditions may present similar symptoms.
In some cases, additional tests or consultations with specialists may be necessary to rule out other potential causes or to assess the severity of the condition. These may include nerve conduction studies, electromyography (EMG), or consultations with neurologists or orthopedic surgeons.
Early and accurate diagnosis of spinal stenosis is crucial for implementing timely and effective treatment strategies. If you suspect you may have spinal stenosis or are experiencing symptoms consistent with the condition, it is recommended to seek medical attention to undergo a comprehensive evaluation and obtain a proper diagnosis.
4. What are the different types of treatment for spinal stenosis
The treatment approach for spinal stenosis aims to alleviate symptoms, improve function, and enhance the quality of life for individuals affected by the condition. The choice of treatment depends on various factors, including the severity of symptoms, the location of stenosis, overall health, and individual preferences. The following are some common treatment options for spinal stenosis:
- Conservative (non-surgical) treatments:
Conservative treatments are usually the first line of management for spinal stenosis and may include:
- Physical therapy: A structured exercise program guided by a physical therapist can help strengthen the supporting muscles, improve flexibility, and enhance overall spine stability. Physical therapy may also include modalities such as heat or cold therapy, ultrasound, or electrical stimulation.
- Pain management: Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or prescription medications may be used to manage pain and reduce inflammation. In some cases, corticosteroid injections may be administered to alleviate symptoms and provide temporary relief.
- Assistive devices: The use of assistive devices like canes or walkers can help improve balance and reduce the strain on the spine while walking. Back braces or corsets may also be recommended to provide additional support.
- Lifestyle modifications: Making certain lifestyle changes, such as maintaining a healthy weight, practicing good posture, and avoiding activities that exacerbate symptoms, can help manage spinal stenosis and prevent its progression.
- Surgical options:
If conservative treatments do not sufficiently alleviate symptoms or if the spinal stenosis worsens, surgical intervention may be considered. The specific surgical procedure recommended will depend on the location and severity of the stenosis. Some common surgical options include:
- Laminectomy: This procedure involves removing a portion of the vertebra or the entire lamina to create more space in the spinal canal and relieve pressure on the spinal cord or nerve roots.
- Spinal fusion: In cases where there is spinal instability, spinal fusion may be performed. It involves fusing two or more vertebrae together, providing stability and reducing pressure on the nerves.
- Foraminotomy: This surgical procedure aims to widen the openings through which the nerve roots exit the spine, relieving pressure and reducing symptoms.
- Interspinous spacer: An interspinous spacer is a small device inserted between the vertebrae to maintain the space and alleviate pressure on the nerves.
The decision to undergo surgery is typically made after a thorough evaluation and discussion with a healthcare professional, taking into consideration the risks, benefits, and potential outcomes.
It is important to note that treatment for spinal stenosis should be individualized based on the unique needs of each patient. Consulting with a healthcare provider specializing in spinal conditions is essential to determine the most appropriate treatment plan for your specific situation.
5. Where to find more information
| Resource | Link |
|---|---|
| Mayo Clinic | Visit website |
| Spine-health | Visit website |
| American Association of Neurological Surgeons | Visit website |
| National Institute of Arthritis and Musculoskeletal and Skin Diseases | Visit website |
| Spine Universe | Visit website |

Anthony Maritato, PT
Physical Therapist
Anthony Maritato, PT has been a licensed physical therapist and private practice owner since 2006. Ohio license #PT011602.
Anthony has been passionate about helping patients recover from total knee replacement surgery as well as rotator cuff repair surgery.

Total Knee Replacement Pre Surgery Online Class
This total knee replacement class is 100% online, and totally FREE. In this three part class you will learn what to do 6-weeks before your surgery, the day of surgery, and 12-weeks after surgery.* Class Dates To Be AnnouncedFREE Online Knee Replacement Pre-Surgical...

Can you use a TENS unit after knee replacement?
TENS is a safe and effective way to reduce pain after a total knee replacement. Transcutaneous Electrical Nerve Stimulation also known as TENS offers a way to reduce pain without medication. TENS may be used during knee range of motion exercises as well as while icing...

How To Stretch A Stiff Knee After Knee Replacement
Is it Safe to Stretch a Stiff Knee It is important to understand what may be causing knee stiffness before stretching the knee. After total knee replacement, the most common cause of knee stiffness includes edema, scar tissue formation, and reflexive guarding due to...
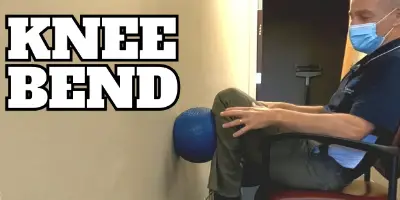
Knee Replacement Bending Flexion Exercises at Home
Knee bending exercises, also called knee flexion, may be performed at home immediately following knee replacement surgery. Heel slides are the most common form of knee flexion exercise. In this video, you will learn more advanced knee flexion exercises to perform at...

Can I Run After Knee Replacement
Conventional advice is to avoid high impact activities after a total knee replacement. This would include running, jogging, and other high impact sports. The concern is the increased wear and tear on the new knee will cause it to wear out sooner or possibly even...

How soon after knee replacement can I use exercise bike?
You can start using an exercise bike within the first 48-hours following a knee replacement surgery. Standard practice in many physical therapy clinics is to begin using a recumbent bike with a gentle rocking motion until the knee is capable of a completing full...

Calf Pain After Knee Replacement
Calf and thigh pain is common after a total knee replacement. Calf pain may be caused by sore muscles due to increased swelling, altered walking mechanics, limited range of motion, and performing new exercises like ankle pumps and heel slides.Tight Calf Muscles After...

Minimalist Running Shoe Review Unboxing Merrell Men’s Trail Glove 4 Runner
Minimalist Running Shoe Review Unboxing - Merrell Men's Trail Glove 4 Runner The Merrell Men's Trail Glove 4 Runner has been a great show. I am updating this description today January 1, 2020. I have worn the shoe for work in the clinic as a physical therapist as well...

Best Tip To Improve Knee Extension- Prone Hangs
Best Tip To Improve [Knee Extension] After A Total Knee Replacement - Prone Hangs - PT at home 2020Swelling, pain, and other factors may contribute to limited range of motion in both extension and flexion. The most effective way to improve knee extesion is to perform...